Abstract
Background
An increasing number of patients (pts) requiring anticoagulation are treated with oral factor Xa inhibitors (DOAC) as an alternative to vitamin K antagonists. Prior to the recent approval of coagulation factor Xa (recombinant), inactivated-zhzo in May 2018, four factor prothrombin complex concentrates (4PCC) have been used to reverse the effects of DOACs. We retrospectively analyzed our institutional experience with 4 PCC for reversal of apixaban and rivaroxaban to determine the indications for 4PCC use and outcomes.
Methods
After IRB approval, pts receiving 4PCC, from Feb 2016 to January 2018 were identified from our pharmacy database and pts receiving PCC for reversal of apixiban and rivaroxaban were selected. Consenting pts medical records (MR) were reviewed for demographics and indications for DOAC and 4PCC as well as outcomes of 4PCC use. Pts were excluded if they had discontinued DOAC greater than 7 days before receiving 4PCC or if they were started on alternative forms of anticoagulation at a therapeutic dose prior to receiving PCC.
Primary endpoint was clinical efficacy (clinical improvement or stability) or ability to undergo required procedure) and secondary endpoint was safety (thromboembolism and death) up to 35 days post-infusion of 4PCC. Stability for intracranial hemorrhages (ICH) was determined by clinical improvement and if head imaging performed, no change in head CT or MRI scan, whereas stability for other bleeds was determined by hemoglobin stability and opinions of providers in the MR. Primary efficacy outcome for pts undergoing surgery was based on MR comments by the performing surgeon and use of other hemostatic agents and red blood cell transfusions.
Results
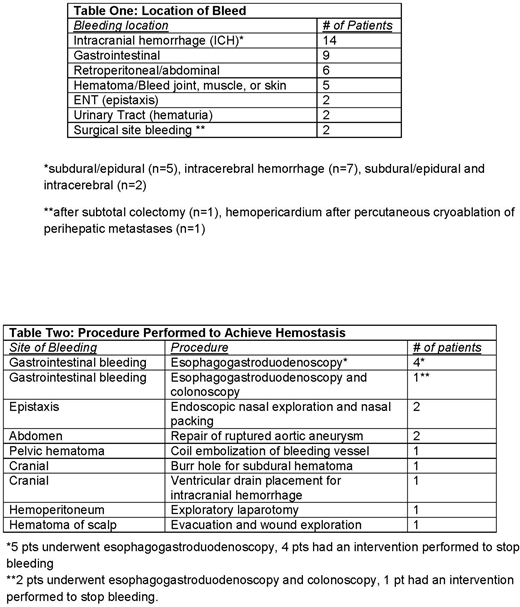
49 (32 male) pts, median age of 74 (31-95) years, met our study criteria and received 4PCC for reversal of apixaban (n=29) and rivaroxaban (n=20). Indications for anticoagulation were atrial fibrillation (n=35) and thrombosis (n=14). Of the 14 pts with thrombosis, 11 had deep vein thrombosis while 3 had thrombosis at other sites (arterial graft thrombus, aortic thrombus, and portal vein thrombosis). 4PCC was administered in the emergency department (n=36), intensive care unit (n=10), or the general medical wards (n=3). Indications for 4PCC included bleeding (n=40), procedure/surgery (n=6), and hemodynamic instability with clinical suspicion for bleeding (n=3). Bleeding location is reported in table 1. All procedure/surgery performed for clinical symptoms not related to hemorrhage were non-elective procedures and included exploratory laparotomy (n=4), laparoscopic cholecystectomy (n=1), and incision and drainage of abdominal wall abscess (n=1). Median PCC dose was 42 (10.3-63.3) IU/kg.
Outcomes
32/40 (80%) pts had stability or an improvement in bleeding, while 5 pts had bleeding that did not improve. 3 pts, all with ICH, had a bleed that worsened 8 (6-8) hours after PCC but then spontaneously stabilized 24 (8-24) hours later. Of those presenting with clinical bleeding, 3 pts received FFP within 3 hours prior to treatment with 4PCC, 2 pts received FFP within 12 hours after 4PCC, and 2 pts received FFP within 3 hours before and 12 hours after 4PCC. Of 40 pts receiving PCC for bleeding, 14 also had a procedure to help achieve hemostasis (Table 2).
All 6 pts were able to undergo procedure/surgery. 5/6 patients achieved adequate hemostasis. One pt had no mention of unanticipated bleeding in the MR but received 8 units of FFP intraoperatively after 4PCC.
6/49 (12%) pts had a thrombotic complication within 35 days of receiving PCC (median 4 days; (range 1-31) including arterial graft thrombus (n=1), superficial venous thrombus (n=1), bilateral soleal vein thrombosis (n=1), internal jugular vein and innominate vein thrombosis (n=1) stroke (n=1), and progression of preexisting portal vein thrombosis (n=1). All-cause mortality was 20%. 3/10 deaths were in pts who never achieved neurologic recovery after ICH and one pt had stroke-like symptoms leading to death 30 days after 4PCC (administered for ICH).
Conclusion
In this cohort, 80% of pts demonstrated clinical stability/improvement of hemorrhage. All pts were able to undergo surgical procedures; however 17% required additional FFP to achieve hemostasis. Thromboembolism occurred in 12% of patients. No deaths could definitely be attributed to 4PCC; however, 30% of deaths could be attributable to the underlying hemorrhagic episode.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal